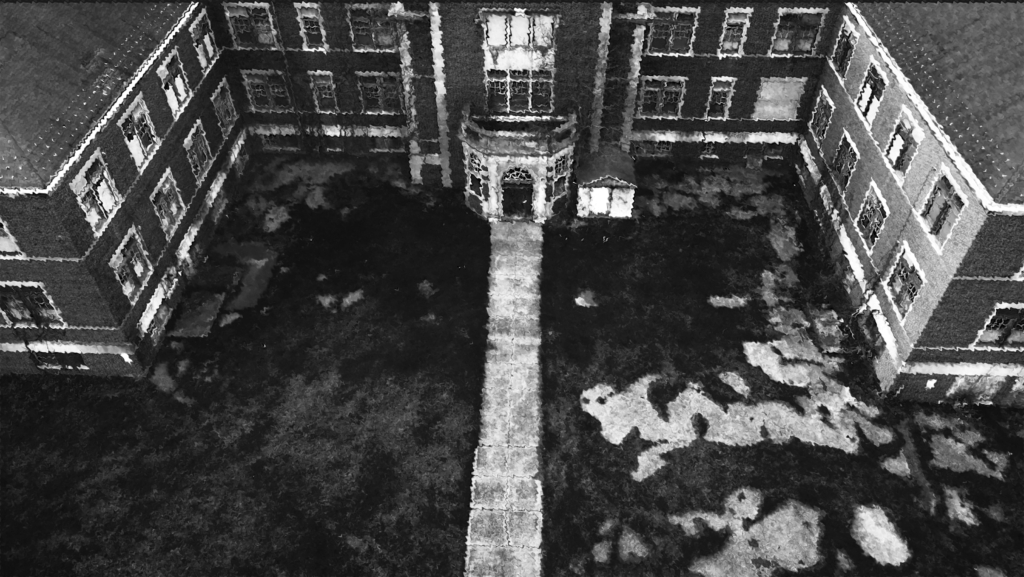
Pennhurst Asylum History
The history of Pennhurst Mental Asylum is marked by not only its founding ideals but also its tragic descent into abuse and unethical practices. Opened in 1903, the asylum was initially seen as a beacon of hope for those suffering from mental illness. However, from the 1920s to the early 1940s, the institution became infamous for conducting dangerous experimental procedures on its patients, particularly on vulnerable individuals.
In the years following World War I, advancements in psychiatric treatment led some institutions, including Pennhurst, to explore experimental therapies. These procedures often prioritized research and institutional goals over patient safety and ethical considerations. Among the most controversial practices were lobotomies, electroconvulsive therapy (ECT), and various forms of aversion therapy, which were performed with minimal oversight or consent.
Lobotomies, a surgical procedure that involved severing connections in the brain’s prefrontal lobe, gained popularity during this period as a means of treating severe mental illness. While proponents claimed it could alleviate symptoms of psychosis and depression, many patients were left with debilitating side effects, including personality changes, cognitive impairments, and emotional numbness. Pennhurst, like many other institutions, adopted this practice, often without adequately informing patients or their families.
Additionally, electroconvulsive therapy was used as a treatment for a wide range of conditions, often administered inappropriately and without proper monitoring. The use of ECT in its early forms was particularly crude, with little regard for patient comfort or safety. Patients would frequently be subjected to multiple treatments without thorough evaluations, leading to further psychological and physical harm.
Another alarming aspect of Pennhurst’s history during this period was the implementation of aversion therapies, which aimed to condition patients away from unwanted behaviors through painful or distressing stimuli. These methods included the use of electric shocks or other forms of punishment, often on children who were already in a vulnerable state. Such practices not only failed to address the underlying issues faced by the patients but also inflicted further trauma and suffering.
The consequences of these dangerous experimental procedures were devastating. Many young patients emerged from these treatments more traumatized than when they entered the asylum, raising serious ethical questions about the practices at Pennhurst. The lack of regulatory oversight meant that patients were often treated as subjects in a cruel experiment rather than individuals deserving of care and respect.
As awareness of these abuses grew, the public began to demand accountability and reform. The culmination of these efforts came in the 1970s, when an investigative exposé revealed the extent of the mistreatment and unethical practices occurring within the asylum. This prompted widespread outrage and ignited a movement advocating for the rights of mental health patients.
The asylum eventually closed, though it was not until 1999, when a number of disturbing accusations came to light. Parents of several of the children seeking treatment at the facility reported visible injuries and upon further investigation, both physical and mental abuse was uncovered. Not long after the abuse came to light, the state decided to close the hospital, but it was not before another tragedy would befall its walls. The hospital was thrown into the national spotlight following reports a thirteen-year-old-girl had gone missing as staff was preparing to take her back to her parents.
To this day, Pennhurst’s legacy serves as a stark reminder of the potential for abuse in mental health care when ethical standards are disregarded. Today, it highlights the importance of informed consent, patient dignity, and the need for a compassionate approach to mental health treatment.
In reflecting on Pennhurst’s history, we are reminded of the lessons learned from its past: the critical importance of safeguarding the rights of vulnerable populations and ensuring that mental health care is delivered with respect, compassion, and a commitment to ethical standards.